Chemotherapy
Chemotherapy drugs given orally or intravenously, kill cancer cells. However, they can harm normal cells too and this can cause side effects. There are potential side effects of chemotherapy, discuss with your oncologist so that you can manage the side effects better2.
Radiotherapy
Radiotherapy is the use of high-energy radiation that kills cancer cells. Radiotherapy may be given to control your cancer and also used to relieve bone pain. It is common to radiate metastases in the bone that are causing pain2.
Radiotherapy for metastatic breast cancer is usually given as a single dose or as a short course over a few days. You may experience skin irritation, tiredness, aches and swelling on the treatment areas.
Anti-hormonal drug therapy
Estrogen and progesterone are hormones that cause some breast cancer cells to make more cancer cells. Estrogen is mostly made by ovaries and made in small amounts by the adrenal glands, liver and body fat. Progesterone is mostly made by the ovaries. Blocking these hormones from working or lowering hormones levels may help stop breast cancer cells from growing2.
There are two classes of hormonal therapy which are Antiestrogen and Aromatase inhibitor.
| Hormonal therapy | Generic drugs name |
| Antiestrogen | Tamoxifen
Fulvestrant |
| Aromatase inhibitor | Anastrozole
Letrozole
Exemestane |
Hormone therapy may cause menopause-like symptoms. Menopausal symptoms include hot flashes, vaginal discharge or dryness, sleep problems, weight gain, thinning of hair, fatigue and changes in mood6.
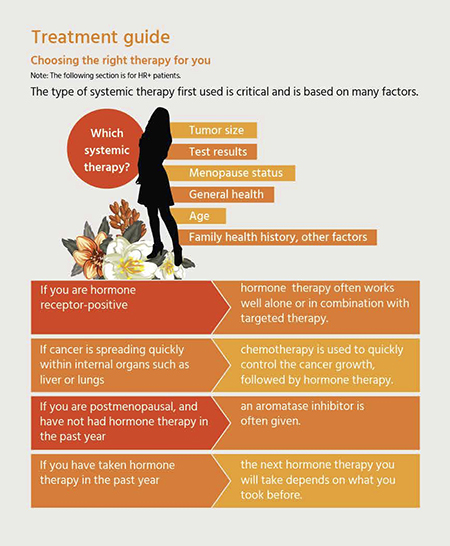
Targeted drug therapy
Targeted therapies work on specific types of breast cancer by blocking specific pathways that breast cancer cells use to multiply. To determine if any targeted therapies are right for you, your oncologist will have to determine what type of cancer you have2.
There are therapies which are used in the treatment of HR-positive breast cancer that specifically target the signaling pathways that are activated by hormones, such as estrogen2.
There are also several therapies that target HER2 receptors2. These drugs work in people with high levels of HER2 in the cancer cells, but they do not work in cancers that do not have this protein.
| Subtype7 | Generic drugs name7 |
| HER 2+ | Trastuzumab
Lapatinib
Pertuzumab
Ado-trastuzumab emtansine |
| HER 2- | Bevacizumab |
| HR+ / HER2- | Everolimus
Palbociclib
Ribociclib |
Bone stabilizing agents
These are drugs that are often used when there are metastases in the bone. They work by helping to strengthen your bones and help reduce bone loss.
They can help relieve bone pain and reduce the long-term risk of bone breaks3. They are taken as pills or injections.
Surgery
Surgery is rarely used in metastatic breast cancer2. When it is used, it is because removing tumor tissue will help to improve your body function or relieve pain.
If you have surgery, you may receive drug therapy and/or radiotherapy.